Executive Summary
Baylor Foundation Uganda is delighted to have been selected to participate in the response against the Sudan Ebola virus disease (SUDV) that broke out on September 20, 2022. Together with assistance from development partners and in collaboration with other implementing partners, we stepped up efforts to prevent, detect, and respond to the public health emergency that began in the Mubende and Kassanda districts and eventually spread to the districts of Bunyangabu, Jinja, Kagadi, Kampala, Kyegegwa, and Masaka, as well as the four high-risk non-response districts of Kakumiro, Kyenjojo, Kabarole, and Mityana. During our four-month involvement, we implemented various strategies, such as SUDV situation rooms/Data Center, to provide timely situation updates. We further seconded staff to the Ministry of Health (MOH) Incident Management Team and the National Public Health Emergency Operations Centers to support epidemiology, surveillance, public health emergencies, health informatics, and the development of alert management systems (AMS) to guide tailored response efforts at both district and national levels.
Additionally, we improved surveillance response efforts to support contact tracing, active case search for sick persons and suspected SUDV alerts, point of entry (PoE) screening at border points, community-based disease surveillance, and mortality surveillance. We further assisted 489 healthcare facilities to implement SUDV IPC/WASH (Infection Prevention and control / Water, Sanitation and Hygiene) and further trained 138 laboratory personnel and 154 drivers across five districts on safe SUDV specimen collection and transportation from contacts, confirmed cases, and dead bodies.
Our collaborative efforts enabled Uganda to contain the virus within a record four months. Even after this remarkable accomplishment, it was necessary to follow up the Ebola survivors. With support from the United States Agency for International Development (USAID), the Ministry of Health in partnership with Baylor Foundation Uganda, established the National Ebola Survivors’ Program, the first of its kind in Uganda. This program has been instrumental in providing mental health, psychosocial support, and clinical care to Ebola survivors to support their full recovery from the after-effects of the Ebola virus disease and address stigmatization and discrimination in their communities.
This initiative has so far managed to prevent a resurgence of the disease that resides in the immunological sites of men and nursing mothers. We express our gratitude to USAID for facilitating the tracking of the Ebola virus’ persistence in these survivors, with 95% of them turning negative by December 2023. The program is currently being funded by Centers for Disease Control and Prevention.
Introduction
The Ministry of Health (MOH) Uganda established the National Ebola Survivors Program with assistance from Baylor Foundation Uganda and with funding from the United States Agency for International Development (USAID) on November 1, 2022. The aim of the program was to provide high-quality medical care, mental health, and psychosocial support services to Ebola survivors at established survivor clinics. The clinics also provided nutritional support to infants below 2 years of age who are children of Ebola survivors.
These clinics are located at Mubende Regional Referral Hospital, Entebbe Regional Referral Hospital and Kikandwa HC III and are being run in collaboration with other health implementing partners to facilitate the survivors’ full recovery.
The National Ebola Survivors’ Program currently provides general and specialized medical care to Ebola survivors to address short and long-term health problems to address various effects of the Sudan Ebola virus (SUDV). These survivors include men, women, lactating mothers and children who have been affected by the virus. The program is also addressing the risk of the Ebola virus disease (EVD) resurgence by providing sexual-risk reduction counseling and access to viral persistence testing for semen and breast milk among men and breastfeeding mothers, respectively.
Additionally, the program is providing psychosocial support to EVD survivors and their families to enable them cope with post-EVD trauma, as well as community stigma and discrimination. To help them fully recover, the program has trained community resource persons and survivors to provide continuous counseling support to EVD survivors.
Exploring the Journey of the National Ebola Survivors’ ProgramNakato Norah*(not real name) is a 19-year-old sex worker from the Ndaiga landing site in Kakumiro district. She had seen and briefly heard health workers talking about a medication that prevents sex workers from contracting HIV, but thought it was a hoax. When one of her clients sexually assaulted her, Norah turned to the only option she had heard of: the pre-exposure prophylaxis (PrEP) service available at Ndaiga Health Centre III.
Norah had shunned this information because she thought it was too expensive for her, a single mother struggling to fend for her three children. At the landing site, most young girls have gotten pregnant and opted to engage in transactional sex because they consider it to be one of the quickest and easiest ways to make money. “I found it better than washing people’s clothes or running errands. All I must do is block out any emotions. On a bad day, I get clients who pay between $5 and $10 for each sexual encounter,” Norah intimates.
When she arrived at the health facility and explained her dilemma to the health worker, the health worker explained that PrEP is a daily medication that reduces the risk of contracting HIV, dispelling her misconceptions surrounding the drug. She further reassured her that it was free at government health facilities. To address self-stigma, she explained to Norah that PrEP is not only for sex workers but for everyone who is at high risk of contracting HIV. With that information, Norah felt relieved. “I now have a better and bigger reason to start taking PrEP. I do not want to get HIV. I also do not want to be the reason any other child I get catches it,” beamed Norah, who still has dreams of getting married one day.
As long as Norah stays on PrEP, she—and other sex workers using this comprehensive HIV prevention—can stay HIV-negative with a chance to pursue their life goals. After starting the PrEP medication, Norah realized the importance of protecting herself from HIV and other sexually transmitted infections by taking PrEP. She now actively encourages her fellow sex workers to also consider taking PrEP to stay HIV-negative. Her experience has further helped health educators address the myths and misconceptions about PrEP through targeted messaging.
“Before starting PrEP, I relied on condoms for protection during sexual encounters. Now, I have a sense of liberation during intimate moments. The fear that used to accompany sexual encounters became a thing of the past.” Norah narrated.
Baylor Foundation Uganda, with funding from the U.S. Centers for Disease Control and Prevention, continues to seek out people living in densely populated, underserved areas such as the Ndaiga landing site who are at high risk of contracting HIV. It provides them with the means to safeguard themselves and lead safe and healthy lives. Through targeted messaging aimed at addressing myths and misconceptions about PrEP, there has been an increase in the uptake of PrEP services among key and priority populations from 1,551 clients in December 2023 to 2,070 clients in March 2024.
Story compiled & edited by Honorata Twebaze & Louisa Kiggwe (Communications team at Baylor Foundation Uganda)
On June 11, 2024, Baylor Foundation Uganda welcomed the new CDC Uganda Director Dr. Adetinuke (Mary) Boyd on her inaugural field visit to the Mubende district to monitor CDC-supported programs. She visited Mubende Regional Referral Hospital’s (RRH) HIV clinic, antenatal clinic, maternity ward, Ebola survivor clinic, and the Regional Emergency Operations Center (REOC). The REOC was established with support from the Korean Foundation for International Health (KOFIH), and its operations are supported by the GoU and US CDC through the G2G grant and BFU. CDC support has enhanced the capacity of the team to manage the REOC.
Dr. Cordelia Katureebe Mboijana, the National Coordinator for HIV Care and Treatment and the CDC Cooperative Agreement at the Uganda Ministry of Health AIDS Control Program, expressed gratitude to the CDC for their support in Uganda. She emphasized the Ministry’s supervisory role in public health through Mubende RRH and lauded the hospital’s leadership for their efficient role. “I congratulate Dr. Emmanuel Batiibwe, the Hospital Director, for implementing the program that ensures the hospital’s commitment to its public health responsibilities in the region,” she said.
Dr. Mary Boyd commended Mubende Regional Referral Hospital and Baylor Foundation Uganda (BFU) for their outstanding leadership, data-driven approaches, excellent care, and unwavering dedication to delivering quality healthcare and managing the Ebola crisis. “These qualities are pivotal for becoming a center of excellence. I encourage you to continue this path to guarantee that services reach all communities,” she noted.
Furthermore, Dr. Boyd visited the drop-in center and the DREAMS safe space, both dedicated to HIV prevention with support from PEPFAR through CDC and implemented by the BFU Fort Portal-Mubende mechanism.

Dr. Denise Birungi, the Director of Programs representing the Executive Director of Baylor Foundation Uganda, stated, “The comprehensive approach of the Fort Portal-Mubende mechanism implemented by BFU as the main CDC partner in the region will enhance our ability to provide treatment services to all communities within the region, and we anticipate improved health outcomes in the targeted districts.”
In her closing remarks, Dr. Boyd expressed gratitude for the enduring impact of the American people’s support in Uganda, affirming, “We shall continue to support you, and I eagerly await the celebration of our joint accomplishments.”
L-R; Rosemary (Hoima District HIV FP), Dr. Betty Nsangi, Magambo Samuel (ACAO Buliisa) Joy (YPLHIV) & Felix Mugano (Hoima City Health Officer) display their lit candles at the National Candlelight Memorial commemoration event at Boma Grounds, Hoima City.
Baylor Foundation Uganda (BFU) joined the Uganda AIDS Commission (UAC) and Bunyoro region stakeholders to review the Presidential Fast Track Initiative (PFTI) performance report and commemorate the International Candlelight Memorial, in Hoima City. The International AIDS #CandlelightMemorialDay is an event that honours lives lost to and affected by HIV and AIDS. The national event was held under the theme: “Ending the AIDS epidemic by 2030: Keeping communities at the center.”
Dr. Betty Nsangi, the Project Manager of the PEPFAR-funded ACE-Bunyoro mechanism implemented by BFU with support from CDC, presented the regional PFTI performance report at the stakeholders’ meeting that preceded the national event. The report enlightened the stakeholders about the region’s progress in HIV implementation and identified areas of improvement in the country’s bid to end the AIDS epidemic by 2030.


L-R: Dr. Betty Nsangi, Ms. Mary Borgman (PEPFAR Country Coordinator, Ms. Jacqueline Makokha (UNAIDS Country Coordinator and Dr. Dirisa Musiisi (CDC Programming Advisor and Lead Activity Manager for the BFU Bunyoro Mechanism) in a photo moment. Dr. Betty shares a light moment with Hon. Jennifer Namuyangu (State Minister for Bunyoro Affairs) at the stakeholders’ meeting ahead of the National Candlelight Memorial commemoration event in Hoima.
In her remarks, PEPFAR Country Coordinator, Ms. Mary Borgman noted that Uganda ranks 5th in countries contributing to new HIV cases in the world despite all the investments and interventions implemented. She pledged continued PEPFAR support to mechanisms such as the ACE-Bunyoro to ensure Uganda achieves HIV epidemic control.
The UNAIDS Country Director, Ms. Jackline Makokha noted that it is expected that by 2030, all countries will have made efforts to end AIDS as a public health threat and achieve epidemic control. She urged BFU, which is currently the comprehensive U.S. CDC implementing partner in the region to support the districts to delve into the inequalities in access to and availability of HIV services in the region.
The commemoration of the Candlelight Memorial event was a significant highlight, where various leaders reiterated the coordinators’ remarks from the stakeholders’ meeting and appreciated BFU for its consistent engagement with the regional leadership to end the AIDS epidemic by 2030, demonstrating remarkable accountability.
According to the UN Resident Coordinator Susan Namondo Ngongi, overlapping inequalities, such as those of gender and socioeconomic status, exacerbate the HIV situation and high rate of teenage pregnancies. “We must deliberately reach vulnerable girls with prevention services and information “, she stated. She also emphasized that new infections are a setback to the progress achieved, necessitating continued efforts to combat any new cases.
Dr. Felix Mugano, the Hoima City Health Officer, representing the DHOs in the region, attributed the increasing infection rates to the influx of people drawn to the region by oil exploration, fishing, and the surge in plantation labour.
Speaking on behalf of the US. Ambassador to Uganda, Ms. Mary Borgman highlighted “PEPFAR has focused on community-led monitoring to identify barriers to accessing HIV services and implementing innovative solutions.”

The Chief Guest, Hon. Milly Babirye Babalanda, the Minister for the Presidency, urged Ugandans to consistently work towards ending AIDS, not only on commemorative days but every day. She stressed the role of communities in achieving the goal of ending AIDS by 2030. She also tasked the oil construction companies to put social safeguards and work with district leadership to avoid being the source of new HIV infections.
ABOUT BAYLOR FOUNDATION UGANDA
Baylor Foundation Uganda is a leading provider of high-quality, person-centered integrated, comprehensive HIV, tuberculosis (TB), reproductive maternal, neonatal, child, and adolescent health (RMNCAH), and global health security services. Established in 2006 as an indigenous, not-for-profit organization, Baylor Foundation Uganda aims to provide high-quality family-centered health care, education, and research to reduce morbidity and mortality from infectious and non-communicable diseases and maternal and childhood conditions.
Baylor Foundation Uganda has scored highly on the Division of AIDS (DAIDS) laboratory quality standards for HIV/AIDS research following a successful laboratory general audit by the Pharmaceutical Product Development (PPD) under the international Thermo Fisher Scientific company. This achievement makes Baylor one of the few trusted laboratories worldwide to be approved by the DAIDS Clinical Laboratory Oversight Team (DCLOT) to conduct high quality inferential research on HIV/AIDS under the HIV Prevention Trials Network (HTPN) and the International Maternal Paediatric Adolescent AIDS Clinical Trials (IMPAACT) network.
This is the second time the DCLOT has contracted PPD under Thermo Fisher Scientific to audit the laboratory following an assessment that approved the laboratory to conduct DAIDS research studies—a major breakthrough for the laboratory. This audit aimed to evaluate its adherence to the DAIDS guidelines for Good Clinical Laboratory Practice (GCLP) standards and identify any opportunity for improvement. The report also stated that the laboratory’s documentation, practices, and record-keeping were exceptional, further demonstrating their commitment to quality. Overall, the audit results reflect positively on Baylor Foundation Uganda’s reputation as a reliable and efficient research facility.
According to Mr. Peter Oballah, the Laboratory Manager, Baylor Foundation Uganda’s commitment to quality assurance has enabled the laboratory to continue contributing valuable data to inferential research studies under IMPAACT and HPTN to advance scientific knowledge and improve patient outcomes. Mr. Oballah also highlighted the importance of ongoing training and collaboration with other research institutions to ensure the laboratory remains at the forefront of scientific advancements. ‘This dedication to excellence has solidified Baylor Foundation Uganda’s reputation as a trusted partner in global health research efforts,’ he said.
“These successful PPD audit results are evidence that our laboratory is consistently meeting and exceeding internationally acceptable health standards for quality and safety, including accuracy and reliability,” Mr. Oballah stated confidently. This recognition further validates our commitment to quality and precision in all aspects of our work. “We are proud to be recognized for our reliability and this achievement should enable Baylor Foundation Uganda to positively influence health policies in Uganda and beyond, ultimately enhancing the lives of children and their families through evidence-based research,” said Dr. Dithan Kiragga, the Executive Director of Baylor Foundation Uganda.
Through the AIDS Support Organization (TASO), the Global Fund Principal Recipient 2 (PR2) for the non-public sector, Baylor Foundation Uganda (BFU) was awarded UGX 7.56 BN for FY 2024 as a sub-recipient (SR) of Grant Cycle 7 (GC7). This funding will support Uganda’s HIV and TB reduction strategy in 38 districts and two cities.
Dr. Denise Josephine Birungi, Head of Programs at BFU said that BFU had been a sub-recipient of the previous grant cycles, NFM (New Funding Model) 2 and NFM3 since 2018. Additionally, she mentioned that this grant will enable BFU to continue its vital work in combating HIV and tuberculosis in these areas, ultimately contributing to the overall health and well-being of the communities served. “This collaboration with TASO will improve health outcomes and reduce the impact of HIV and tuberculosis in populations at high risk. I am confident that together we can make a positive impact on the lives of individuals affected by these diseases by working together to achieve sustainable results,” said Dr. Dithan Kiragga, Executive Director of BFU.

On February 28, 2024, Baylor Foundation Uganda (BFU), welcomed H.E. William Popp, the U.S. Ambassador to Uganda on his debut visit to the Rwenzori region to see the impact of U.S. government health investments in the communities. Baylor Foundation Uganda is currently the comprehensive HIV PEPFAR implementing partner of the U.S. government in the region that includes Kasese, Bundibugyo, Kabarole, Bunyangabu, Kyenjojo, Kyegegwa, Kamwenge, Kitagwenda, Ntoroko districts and Fort Portal City. More recently, Baylor Foundation Ugandaexpanded its scope to include the Fort Portal-Mubende region that encompasses the districts of Mubende, Nakaseke, Kiboga, Kyankwanzi, Kassanda and Mityana, under the CDC-funded Fort Portal-Mubende mechanism. The mechanism aims to accelerate and sustain HIV epidemic control and in collaboration with the Global Health Security program, strengthen border health and disease outbreak response efforts.
For the past 12 years, Baylor Foundation Uganda has received USG funding from the U.S. President’s Emergency Plan for AIDS Relief—PEPFAR through the U.S. Centers for Disease Control and Prevention (CDC), to implement comprehensive HIV/TB plus maternal and child health services in the Rwenzori region including at Fort Portal Regional Referral Hospital (RRH) that the Ambassador also visited.
At Fort Portal RRH, Amb. Popp visited the Neonatal Intensive Care Unit (NICU) that was renovated and equipped with U.S.G support in 2013 under the Saving Mothers, Giving Life (SMGL) project, a USG funded project to improve maternal and neonatal outcomes. He also visited the Public Health emergency Operations Center that is enhancing surveillance for public health threats and emergencies in the region. He was briefed about USG-supported border health activities that are being implemented through active screening and cross border surveillance to quickly detect, respond and contain disease outbreaks within the region given the high cross border interactions.
While interacting with the ART clinic team at the hospital, he emphasized the importance of people testing for HIV/AIDS to know their status. “We want people to get tested for HIV/AIDS to know their status, and these are things that the U.S. government has supported and is supporting with funding from the U.S. PEPFAR program,” he said—adding that those who test positive for HIV and enroll on treatment, experience suppressed viral loads making it unlikely for them to transmit the virus to others. Last year, over 7,500 HIV positive individuals in the Rwenzori region alone were started on antiretroviral treatment. Over 70,000 patients in the area are currently receiving treatment, and 95% of them have attained viral load suppression.
Accompanied by Baylor Uganda Executive Director Dr. Dithan Kiragga—and Baylor Foundation Uganda technical staff; Amb. Popp also visited Bundibugyo Hospital whose laboratory was refurbished and equipped by Baylor Foundation Uganda in 2018 with USG funding. The laboratory has since received SANAS accreditation. Here, he observed integrated laboratory services central to the diagnosis and monitoring of diseases including HIV/TB and outbreaks. He saw how USG support through PEPFAR has enabled the facility to provide accessible and high-quality laboratory services that meet international standards albeit in a remote rural setting. Patients at peripheral sites including hard-to-reach and underserved communities can access this service through a motorbike rider system keeping turnaround time to a minimum.

Dr. Kiragga accompanied Amb. Popp and his entourage to visit the hospital’s Ebola Memorial Cemetery, where the 2007 Bundibugyo Ebola victims (Health Staff) are laid to rest—and paid pay tribute to the fallen heroes.
Dr. Dithan Kiragga, the Executive Director of Baylor Foundation Uganda appreciated the generosity of the American people. “As an implementing partner, Baylor Foundation Uganda appreciates the continued support from the American people, which over the years has saved lives and improved health for many families.,” said Dr. Kiragga.
Overview
Testing for viral load is a globally accepted mechanism for monitoring HIV treatment success and virologic failure among people living with the virus. In 2018, Uganda transitioned from the dry blood spot mechanism to plasma as a measure of the effectiveness of ART. Both the CD4 and viral load processes allow clinicians to determine which client is eligible for initiation on antiretroviral therapy (ART), the disease progression, and treatment response.
 |
Viral load testing for children and adolescents is conducted every six months; pregnant women every three months and adults once every year. Before 2022 revised consolidated guidelines for the prevention and treatment of HIV, viral load blood tests for stable clients were repeated when they have more than 1,000 copies of the virus per ml of blood. In 2022, viral load suppression was reduced to 200 copies of the virus per ml of blood.
Problem
The viral load testing coverage target for the United Nations Joint Program on HIV/AIDS (UNAIDS) is 95 percent of all HIV clients active on ART. However, by October 2021, viral load testing coverage for the Bukedi region, one of the regions for USAID Local Partner Health Services- Eastern (LPHS-E) By Oct 2021 stood at 84 %.
USAID LPHS-E is the main HIV and TB implementing partner in the Bukedi and Bugisu regions. The Activity must facilitate the transportation of samples from the lower health facilities to the hub before they reach the Ministry of Health’s Central Public Health Laboratories (CPHL), says Ronald Mangeni, Laboratory Services Officer for Cluster II, USAID LPHS-E.
By Oct 2021, hub riders delivered only half (50%) of the viral load samples within two days at the hub laboratories for processing using point-of-care testing for Pregnant and breastfeeding women, and transportation of other patients’ samples for processing at the National referral laboratory CPHL in Kampala. Delays were due to sample packaging at the spoke facility, online CPHL hub tracker data was not utilized. The facilities lacked the centrifuges necessary for extracting plasma from the blood sample.
Packaging dry blood spot samples were challenging because they were collected and stored at different points of care at facilities. Sometimes health workers forwarded the samples without request forms. “We often engaged in packaging samples. If we didn’t, we would delay more,” says David Okiria,Hub Rider for Pallisa, Kibuku, and Butebo Districts.
Human resources shortages in laboratories exacerbated the turnaround challenge. Kibuku District Health facilities could have over 100 samples on the clients
 |
clinic day with only one active lab technician to bleed the clients and fill forms. A form filled in by a Clinician is supposed to accompany each sample for testing in the laboratory. Delivering the dry blood spot samples from the facility to CPHL would take on average 10 days, only to be rejected because the samples had been packed without a form.
The facilities lacked refrigerators for keeping the Plasma Viral load samples which can only be stored at room temperature for six hours. In addition, the hubs were not utilizing the online turnaround time (TAT) tracker data to guide them about which facilities required support.
“The viral load situation was not good. We would send approximately 80% of the dry blood samples to CPHL for processing,” says Samuel Erepu, Lab Technician and Viral Load Focal Person at Pallisa General Hospital.
With the dry blood spot, the procedure was to massage the finger, but the health workers rarely cleaned the finger. Patients were happy because little blood was required of them, says Anyodo.
“After pricking the patient, sometimes we would not get sufficient blood in the circle on the DBS card. The lab was overwhelmed. We rarely took notice of these anomalies because we had a human resource challenge. This made Pallisa Hospital’s performance drop,” says Anyodo.
Results of the dry blood spot test would sometimes take close to three months before they were returned because they were taken to Kampala. Every time Grace Aloyet, Community Health Worker at Pallisa General Hospital, Pallisa District got a month’s drug refill, she would ask health workers if her results were back. Sometimes she never got the results. “Whenever I didn’t receive my results, I felt bad. I needed to know how I was progressing,” says Aloyet.
Aloyet got to know that she was HIV positive in 2004. At the time she received an operation because of intestinal TB. A year later, Aloyet received her CD4 results a month after CPHL in Kampala got her blood sample. She was not suppressing at the time. She enrolled in treatment with The AIDS Support Organization (TASO), Mbale City to receive Co-trimoxazole (Septrin®). The same year, she started volunteering at Pallisa General Hospital.
Since CPHL was processing results of all hubs nationally, the turnaround time would sometimes last up to 49 days, depending on the type of sample tested (Plasma or Dry blood spot). The overall turnaround time for viral load results in the region was 25 days in April 2022 against the national target of 14 days.
“The delay process of 11 days was between sample transportation from the spoke facility to hubs at Busolwe and Pallisa hospitals,” says Mangeni.
Strategies
In 2019, CPHL partially decentralized viral load testing services, placing Point of Care (POC) machines on site in 100 hubs countrywide and selected high volume health facilities. Bugisu and Bukedi regions have 18 POC machines that CPHL regularly services.
With support from USAID LPHS-E, the hubs mapped 20 high-volume facilities in Pallisa, Kibuku, Butaleja, Budaka, and Butebo districts, Bukedi sub-region.
Due to the backlog on viral load testing, the facilities followed up with the clients to re-bleed them. However, some patients would have relocated without their contact details or lacked transport to return to the health facility.
“Whenever we reached a client and started counseling afresh, his facial expression communicated enough. It was as though he was saying the health worker doesn’t know what she is doing,” said Anyodo.
The hubs assigned riders to facilities within a 10 km radius to be revisited twice a day or visited on a non-scheduled day in case emergency samples were collected. A hub rider visits a high-volume facility thrice a week. The five study districts of the Bukedi region have two general hospitals, six HC IV and 38 HC III. The CPHL driver visits a hub on the second and fifth day of the week. The hub makes reminder calls to the facility to prepare samples ahead of visit time. USAID LPHS-E facilitated hub riders to work on Saturdays during services improvement campaigns to timely transport samples from Health facilities and Community
“We established a schedule for the riders which LPHS-E and us review weekly using the online CPHL hub rider’s tracker. The riders go because they are being tracked,” says Erepu.
USAID LPHS-E trained the lab team in different quality, and service provision systems and continues to provide technical support on lab quality management. It supports the districts to hold quarterly performance review meetings to identify challenges and share learnings.
The Activity continues to support hubs like Pallisa General Hospital, Busolwe General Hospital with airtime, stationery, and cartridges for printing the results and pays the salaries of hub riders and some other human resource personnel at the hospital. One such staff is a Lab Assistant who helps with human resources issues. It facilitates the lab staff to run the samples. It provides fuel and maintains the hub riders’ motorcycles. LPHS-E collaborates with USAID Regional Health Integration to Enhance Services- Eastern (RHITES-E) to service the hub motorcycle.
USAID LPHS-E mentored us for two weeks about bleeding and extracting plasma for viral load testing. We would follow up with CPHL about the turnaround time. We would mention the amount of blood to be taken to facilitate the extraction of the plasma. says Erepu.
Results
The proportion of plasma samples collected for Viral load in four districts (Kibuku, Pallisa, Butaleja, and Butebo) improved from 29% (511 DBS VL and 209 plasma VL) in April 2022 to 85% (184 DBS and 1,022  plasma VL) in March 2023 against a national target of 60.0% plasma VL. All health facilities in Budaka District still rely on DBS VL due to a lack of centrifuges. The USAID LPHS-E activity is procuring centrifuges for health facilities.
plasma VL) in March 2023 against a national target of 60.0% plasma VL. All health facilities in Budaka District still rely on DBS VL due to a lack of centrifuges. The USAID LPHS-E activity is procuring centrifuges for health facilities.
Hubs like Pallisa General Hospital now do 100 percent plasma. “It is very easy to handle plasma, rather than dry blood spot. The timely response in case there is a need promotes teamwork” says Erepu. “Using plasma has eased my work. It is better than the dry blood spot. The turnaround time has improved client satisfaction. They can now access results in time,” says Anyodo.
The percentage of viral load samples delivered at a hub in two days from 20 facilities increased from 50 percent in April 2022 to 100 percent by mid-May 2022. The partners have maintained the achievements.
“Patients i.e. EID clients and Pregnant and breastfeeding mothers for Viral load testing are enjoying the services. The testing sites are nearby. It is not like it used to be when the samples were taken to Kampala,” says Okiria.
“I am now suppressed. I am very happy about this system [plasma]. It is the best,” says Aloyet.
The overall turnaround time from sample collection to results printing was reduced from 25 days to 18 days close to the national target of 14 days. Further, within three months of improvement activities, on average, hub riders delivered 699/792 (88 percent) viral load samples at hubs in two days. Currently, in May 2023, the overall Viral load result turnaround time from sample collection to results printing is 14 days as per the National target of 14 days.
“When I see things move, it motivates me. We have very many resourceful people who are cooperative. This makes the process shorter,” says Mangeni.
Conclusion
The turnaround time for results improved through cohesive coordination between the health workers and hub riders.
Recommendations
USAID LPHS-E’s adequate logistical support, roll out of CPHL Results Delivery System using SMS/USD, and timely motorcycle maintenance motivate the hub riders and health workers to reduce the TAT for results. Results are sent in batch numbers and no longer get lost.
USAID LPHS-E Activity works with district leaders to provide quality comprehensive HIV and TB services to the community in 15 districts and Mbale City to screen, identify, link, and monitor TB patients at the facility and community levels.
USAID LPHS-E is supporting 191 health facilities in both Bukedi and Bugisu regions through the health systems strengthening approach in partnership with the leadership in the districts and other implementing partners in the region like USAID Regional Health Integration to Enhance Services in Eastern Uganda (RHITES-E), USAID Health Activity, Mbale Regional Referral Hospital under the G2G mechanism and USAID Local Service Development Activity.
The Project provides key interventions in TB programming at the facility and community levels. We have participated in door-to-door screening through the CAST TB campaign, and continue to support systematic contact tracing. Since October 2021, the Project has supported facilities to identify over 6000 TB cases in both Bukedi and Bugisu regions cumulatively.
In collaboration with USAID RHITES-E and districts in the region, USAID LPHS-E has supported the TB sample transportation network which hosts seven lab hubs in Mbale Regional Referral Hospital, Pallisa, Tororo, Kapchorwa, and Bududa general hospitals and Budadiri HC IV.
We support the TB diagnostic and treatment units in the region to submit quality orders for laboratory and TB commodities. In addition, we monitor regional stock and facilitate the redistribution of commodities according to need.
USAID LPHS-E supports health workers to timely monitor TB patients on treatment through prompt follow-up of missed appointments and reminders for drug pick-ups.
We work with CSOs and VHTs to deliver TB drugs to patients in hard-to-reach areas. As a result of these efforts, TB treatment success rate has improved in January 2022 to December 2022 from 88% to 90.7% and from 82.9% to 86.6% for Bugisu and Bukedi regions in the previous calendar year.
USAID LPHS-E supports 17 GeneXpert sites and seven TrueNat and TB Lamp sites to offer molecular TB diagnosis through referral and onsite testing of sputum samples. This support is geared towards improving drug-resistant case identification. The Activity also supports the districts to link patients diagnosed with drug-resistant TB to the treatment site located in Mbale Regional Referral Hospital.
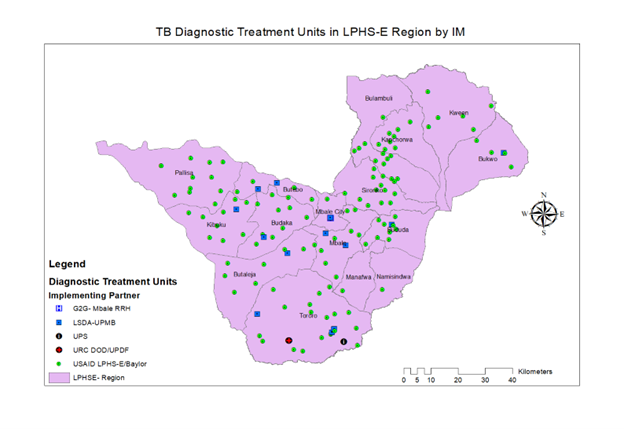
USAID LPHS-E Activity follows the already established QI structures in the country to implement quality improvement initiatives in TB care. Together with the national program and the USAID TB-Activity, LPHS-E supports drug treatment units in the region to participate in the national TB/HIV collaborative activities with the aim of improving TB case detection and treatment outcomes.
The Activity in collaboration with the district health offices supports periodic TB data collection as per the Ministry of Health weekly, monthly, quarterly, and annual schedules. The support extends to monthly and quarterly TB data validation meetings, cleaning, and performance review meetings. The Activity supports the District Health Office (DHO) office to conduct TB data quality assessments to address any data challenges at health facilities.
Kampala, UGANDA: Baylor-Uganda in collaboration with the U.S. Centers for Disease Control and Prevention (CDC) and the Ministry of Health handed over essential maternal and child health (MCH) equipment worth more than $200,000 (UGX800m) to 575 community-level health centers across the country. The equipment included 400 examination beds, 310 examination screens, 425 adult weighing scales, 350 infant weighing scales, 575 BP machines, 800 fetoscopes, and 400 stadiometers.
Baylor-Uganda procured the equipment with funds from the U.S. Emergency Plan for AIDS (PEPFAR). The equipment aims to boost the capacity of the public health centers to improve healthcare outcomes for mothers and children in line with the goal to eliminate Mother-To-Child Transmission (eMTCT) of HIV in Uganda.
“We have procured the right quality of equipment that is needed by the HCIIs, and I believe it will go a long way in contributing to overall maternal and child health outcomes in the country,” said Dr. Leticia Namale, the Director of Health Systems Strengthening at Baylor-Uganda.
According to UNAIDS, Mother-to-Child Transmission of HIV has significantly reduced from 9.46% to 5.85 in 2019. Uganda has not yet attained the 5% WHO MTCT threshold due to sub-populations that still struggle to access MTCT services, mothers who drop off ART, and those that sero-convert later in pregnancy and breastfeeding.
Findings from a recent national PMTCT impact evaluation showed that the majority of pregnant women—nearly half—seek healthcare from lower-level facilities, mostly HCIIs. However, most HCIIs lack the necessary accreditation and equipment to provide HIV antiretroviral therapy (ART)/PMTCT. This means that many pregnant and breastfeeding mothers miss out on critical PMTCT interventions that can prevent HIV transmission to their babies.
Dr. Doreen Ondo, the Program Officer at the Ministry of Health AIDS Control Program stated that although they had accredited 600 HCIIs, ‘their actual capacity to provide HIV ART, PMTCT and Early Infant Diagnosis (EID) services to promptly identify and care for HIV infected infants was still limited. “We decided to procure some basic equipment to aid their work and provide ongoing on-the-job capacity training,” she said.
Dr. Phoebe Namukanja, CDC PMTCT Lead advised the PEPFAR implementing partners present, to collaborate with their local government regional, district and site health teams to ‘ensure that the equipment is well utilized, maintained and accounted for.’
“With this equipment support and our collective efforts, we will ensure that no mother or child is left behind in the journey towards improving healthcare access in Uganda and elimination of mother-to-child transmission—for better, healthier and productive lives,” Dr. Namukanja said.